
x
Recent advancements are transforming the landscape of surgical interventions designed to alleviate joint discomfort and enhance mobility. By refining approaches and focusing on recovery strategies, these developments aim to optimize outcomes and improve the quality of life for individuals seeking relief from knee-related challenges.
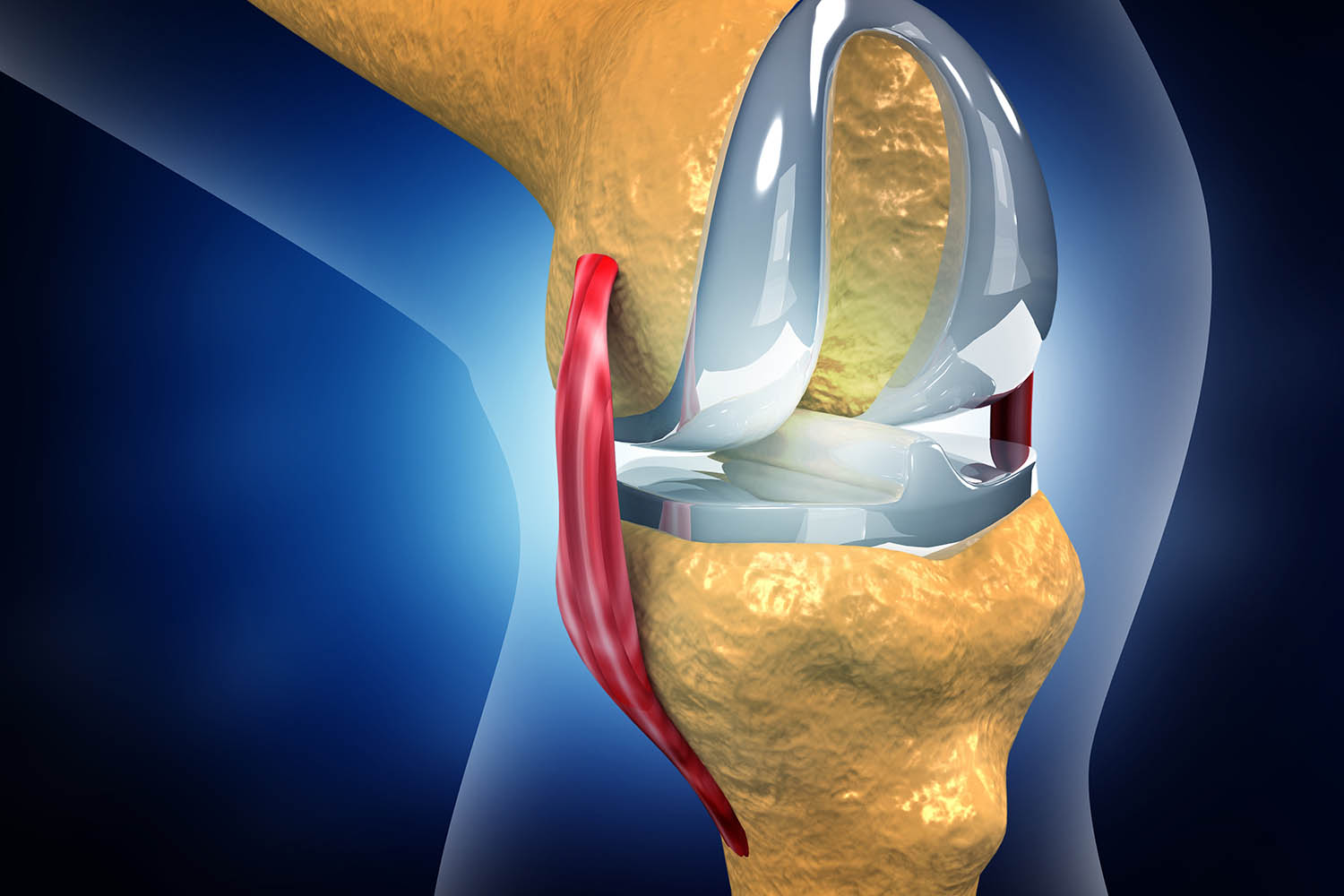
The field of total knee arthroplasty (TKA) continues to evolve, driven by technological innovations and improved surgical methods that enhance patient outcomes. Exploring these advancements reveals a promising future for knee replacement surgeries.
Robotic-assisted surgery in TKA has emerged as a transformative technique, significantly improving the precision of knee replacements. Acting as a tool under the surgeon’s control, robotic systems facilitate meticulous planning and execution. By providing enhanced visualization, these systems guide the surgeon in making precise bone cuts and implant positioning, akin to having a "GPS" for the procedure.
The precision offered by robotic assistance helps ensure better alignment of the knee joint. This can lead to improved joint stability, potentially reducing the risk of implant loosening over time. Moreover, studies indicate that robotic-assisted surgery may lead to less post-operative pain and quicker recovery times. However, more comprehensive research is needed to fully validate these benefits. With these advancements, robotic surgery represents a strategic leap toward optimizing the surgical process, enhancing the long-term success of TKA.
Advances in imaging and 3D printing technologies are moving TKA away from the traditional one-size-fits-all model in favor of patient-specific solutions. This pivotal shift involves the creation of tailor-made implants and surgical instruments that closely fit the unique anatomy of each patient.
Before surgery, detailed imaging captures the intricate structure of a patient's knee. Leveraging this data, engineers design virtual models to create custom-fit implants, ensuring optimal fit and function. Accompanying these are patient-specific surgical guides that aid in achieving precise bone cuts and accurate implant placement. Personalized solutions can lead to enhanced joint function, reduced wear and tear on the implant, and a more natural knee feel post-surgery. While still developing, this personalized approach holds significant promise for the future, potentially transforming patient outcomes in TKA.
Minimally invasive surgery (MIS) has revolutionized various surgical fields, including TKA, aiming to reduce the physical burden of the operation. Incorporating smaller incisions and minimal tissue disruption, MIS offers distinct advantages over traditional open surgery.
Patients undergoing MIS often experience less post-operative pain, reduced blood loss, and shorter hospital stays. Additionally, the smaller incisions typically result in less scarring, contributing to quicker recovery and improved aesthetic outcomes. However, it is essential to recognize that MIS is technically demanding and may not suit all patients. Careful consultation with surgeons is necessary to evaluate the most appropriate approach based on individual patient needs. Ultimately, the aim remains to achieve excellent long-term results with reduced surgical trauma.
The evolution of TKA doesn't stop at surgery; significant advancements are also transforming recovery protocols. A focus on expedited healing aims to enhance the patient experience post-surgery.
Recent developments in rehabilitation prioritize early mobilization and aggressive physical therapy, challenging traditional recovery models. Shifting from prolonged rest to active recovery modalities promotes long-term success.
Early initiation of physical therapy, sometimes within 24 hours of surgery, empowers patients to regain movement more swiftly. Starting therapy earlier facilitates muscle strength improvement, mitigates joint stiffness, and accelerates the return to normal activities. Comprehensive pain management strategies are integrated to enable active participation in these aggressive rehabilitation protocols, allowing patients to embark on their journey to recovery with reduced discomfort.
Effective pain management is pivotal in TKA recovery. Poorly controlled pain can hinder participation in rehabilitation, delaying recovery. The advent of multimodal analgesia represents a breakthrough in addressing these challenges.
By combining various pain medications to target different pathways, multimodal analgesia reduces reliance on opioids, which carry risks of side effects and addiction. Nerve blocks offer another layer of pain relief, providing localized effects to the knee area. These innovative strategies empower patients to actively engage in their rehabilitation, contributing to better surgical outcomes and an efficient recovery process.
Holistic approaches, like combining acupressure with physiotherapy, further enhance pain management during recovery. Acupressure, akin to acupuncture but utilizing pressure, enhances mobility and alleviates pain. Research shows that integrating acupressure with standard physiotherapy results in significant reductions in pain, augmenting the healing process.
By embracing holistic measures, patients experience relief from physical symptoms and enjoy improved overall well-being. Such integrative approaches not only address postoperative pain but also contribute to a smoother recovery journey, paving the way for a more comfortable and effective rehabilitation experience.
The post-operative phase is critical in determining the ultimate success of TKA. Effective rehabilitation is essential for ensuring the long-term benefits of the procedure.
Post-operative rehabilitation extends beyond the knee itself, with a unique focus on strengthening the feet. Strong foot muscles are crucial for balance and stability, significantly impacting overall mobility post-surgery.
The body operates like a chain, where weakness in one area affects the entire structure. Reinforcing foot muscles can lead to notable improvements in balance, reducing the risk of falls and expediting the return to daily activities. Emphasizing foot exercises in rehabilitation plans is a simple yet effective strategy to enhance recovery outcomes, instilling confidence in patients during their recovery journey.
Virtual reality combined with hypnosis (VRH) offers emerging non-pharmacological solutions to manage chronic pain post-TKA. Patients immerse themselves in calming virtual environments while receiving hypnotic suggestions that reduce pain perception.
Studies highlight the significant pain reduction and improved quality of life that VRH can provide. Addressing the psychological facets of pain complements traditional methods, showcasing the strength of mind-body connections in postoperative recovery. VRH underscores the importance of innovation in enhancing surgical recovery experiences.
TKA decisions can be influenced by myths and misconceptions. Separating fact from fiction is crucial for making informed decisions about this life-changing procedure.
Contrary to popular belief, TKA isn't exclusive to older adults. While many recipients are seniors affected by arthritis, younger individuals with conditions like rheumatoid arthritis or injury-related damage can benefit from TKA. Age should not necessarily dictate candidacy; the severity of the condition should guide consideration. If knee pain diminishes life quality, TKA may be an appropriate solution, irrespective of age.
Fears of intolerable post-surgical pain deter some from pursuing TKA. Modern anesthesia and pain control protocols, including regional anesthesia and multimodal pain management, have transformed the post-operative experience. Effective communication with medical teams ensures pain management, fostering a smoother recovery.
What are some current innovations in total knee arthroplasty (TKA) that aim to improve surgical outcomes?
Recent advancements in TKA focus on enhancing precision and personalizing the procedure to improve patient outcomes. One significant innovation is robotic-assisted surgery, which aids surgeons by providing enhanced visualization and precision during bone cuts and implant placement. This can lead to better joint alignment, potentially reducing the risk of implant loosening. Additionally, patient-specific implants and instrumentation, made possible through advanced imaging and 3D printing, allow for a more tailored fit, improving joint function and longevity. These innovations are part of an ongoing effort to optimize surgical techniques and patient satisfaction.
How does artificial intelligence (AI) contribute to advancements in total knee arthroplasty?
AI is becoming increasingly integrated into TKA, assisting in various stages of the procedure. During surgical planning, AI algorithms analyze pre-operative images to help determine the optimal implant size and position. AI can also predict potential complications and suggest tailored rehabilitation programs by analyzing patient data. Moreover, AI-driven wearable sensors and apps monitor recovery progress, providing valuable feedback to both patients and healthcare providers. This technology aims to enhance surgical precision and personalize patient care, ultimately improving outcomes.
What are the benefits of minimally invasive surgery (MIS) in the context of knee replacement?
Minimally invasive techniques in knee replacement surgery focus on reducing incision size and minimizing tissue disruption. The benefits of MIS include less post-operative pain, reduced blood loss, and quicker recovery times. Patients undergoing MIS often experience shorter hospital stays and less scarring compared to traditional open surgery. However, MIS requires specialized skills and may not be suitable for every patient. It's essential to discuss the suitability of MIS with a healthcare provider to weigh its advantages against potential risks.